WHAT IS
ENDOMETRIOSIS
The cause of endometriosis and related pain
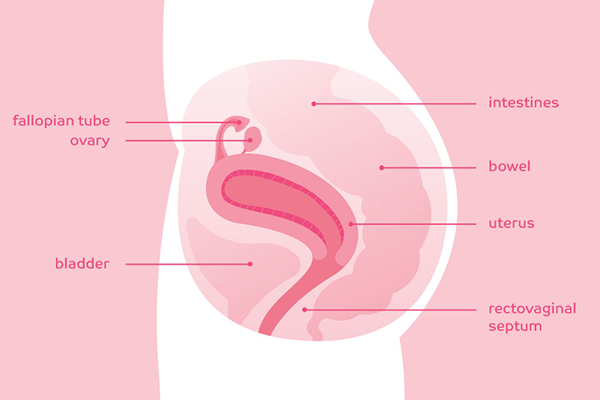
Endometriosis is a chronic and painful disease that occurs when endometrium (tissue that originates from the lining of your uterus) starts growing outside of your uterus, where it doesn’t belong.
The endometrial tissue that grows outside of your uterus is called a lesion or an implant. These lesions are fueled by a sex hormone called estrogen. When estrogen levels rise, these lesions (patches of endometrial tissue) can grow. Later in the menstrual cycle, they may break down and shed. This can cause pain throughout the month.
About endometrial lesions
The location of these lesions can affect your symptoms, but the extent of the disease doesn't necessarily relate directly to
the level of pain experienced.
Common symptoms of endometriosis
Endometriosis is not a “one size fits all” chronic condition and is more than just a “bad period.” In fact, there are many different symptoms of endometriosis. Some women with endometriosis may experience a range of symptoms, while others may experience none at all. Every woman’s symptoms are different.
There are many symptoms of endometriosis, but the most common symptoms are:
- Painful periods: your gynecologist may call this dysmenorrhea (DIS-men-uh-REE-uh)
- Pelvic pain in between periods: your gynecologist may call this non-menstrual pelvic pain
- Pain with sex: your gynecologist may call this dyspareunia (DIS-puh-ROO-nee-uh)
Want to have a more productive conversation with your OB/GYN?
What endometriosis pain treatments exist
To treat your endo pain, your OB/GYN may recommend one or more of the following treatment options:
- Over-the-counter strength painkillers (eg, ibuprofen, acetaminophen, naproxen)
- Prescription strength NSAID painkillers (eg, ibuprofen, naproxen)
- Prescription hormonal birth control (eg, pills, injection, implant, IUD)
- Prescription GnRH antagonist pill
- Prescription GnRH agonist injection or nasal spray
- Prescription androgenic hormones (eg, danazol)
In certain circumstances, your OB/GYN may prescribe opioids (such as hydrocodone with acetaminophen). Another endometriosis treatment option is surgery, such as laparoscopy. There are several different procedures that can treat endo pain. Together, you and your gynecologist will decide which is right for you and your lifestyle.
Want to learn about a treatment option with proven results?
Though the exact cause of endometriosis is unknown, most scientists think it relates to a process called retrograde menstruation. That’s when tissue that lines the inside of your uterus flows out in the wrong direction—through your fallopian tubes—during your period. The out-of-place tissue can cause pain and inflammation as it starts growing on surfaces and organs in your pelvic region.
There are other possible theories as to what can cause endometriosis, such as:
- The immune system not destroying endometrium cells outside of the uterus the way it should
- Metaplasia—where normal cells in the pelvic area change into endometrial cells
- Endometrial cells forming outside of the uterus before birth; during puberty, these cells form endometrial lesions
Some lesions can even form their own nerves or scar tissue (called adhesions) between organs, which can cause pain. Although rare, lesions are sometimes found in areas farther away from the pelvic area.
